Imagine a life completely realigned by pancreatitis, a condition characterized by the inflammation of the pancreas. “Navigating Life with Pancreatitis: An Intimate Look at Swelling of the Pancreas” gives you an intimate journey through the many challenges and changes that shapes your everyday life when battling this condition. Chronic or acute in nature, pancreatitis can drastically curtail your life, peppering your daily routines with doctor visits, change in diet, and relentless pain management. Nonetheless, hope remains. This personal, deeply detailed account provides a guiding light for those affected – offering strategies for coping and inspiring resilience and will to endure.
Understanding Pancreatitis
Coming to terms with a diagnosis of pancreatitis, or swelling of the pancreas, can be daunting. In order to fully grapple with this condition, a comprehensive understanding of it is necessary.
Definition of Pancreatitis
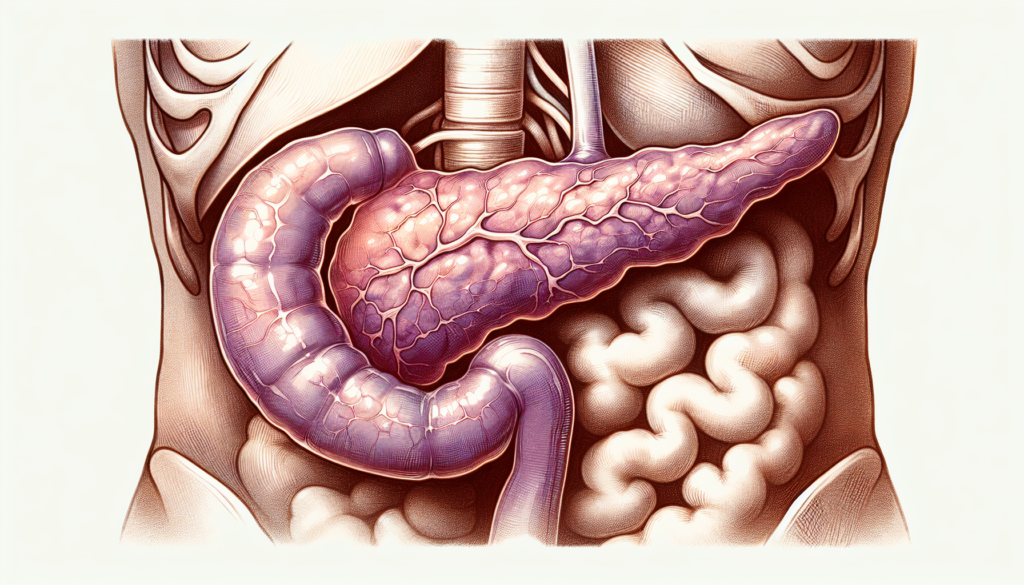
Pancreatitis refers to the inflammation of the pancreas. The pancreas is a critical organ in the human body that assists in digestion and hormones regulation, such as insulin, which controls our blood sugar. When it swells or becomes inflamed, this results in the condition known as pancreatitis.
The Pancreas: Function and Location
The pancreas is a flat organ located in the abdomen, tucked behind the stomach. Its primary functions are to produce enzymes that aid in the digestion of food and to produce hormones that help regulate blood sugar levels. When working correctly, it releases enzymes into your small intestine to help break down food. But, when it doesn’t, we run into problems such as pancreatitis.
Types of Pancreatitis: Acute and Chronic
There are two primary types of pancreatitis: acute and chronic. Acute pancreatitis is sudden and may last for a few days, whereas chronic pancreatitis lingers for many years. Acute pancreatitis can lead to chronic if not appropriately managed.
Causes and Risk Factors of Pancreatitis
Having a deeper understanding of the potential causes and risk factors can give you a clearer picture of what might have led to the development of your pancreatitis.
Alcohol and Gallstones: Leading Causes
Excessive alcohol use and gallstones are the leading causes of pancreatitis. Gallstones can block the pancreatic duct, leading to inflammation, while alcohol can cause the pancreas to produce toxic substances that instigate inflammation.
Other Risk Factors
Other risk factors include heavy smoking, high calcium or triglyceride levels in the blood, certain medications, and certain infections. It’s also worth noting that injury to the pancreas or abdominal area can cause pancreatitis.
Genetics and Pancreatitis
There’s also a proven genetic link in some cases of pancreatitis. Certain genetic mutations can lead to the development of the condition, and it often runs in families.
Symptoms and Signs of Pancreatitis
Identifying the symptoms of pancreatitis can be crucial in seeking timely medical intervention.
Acute Pancreatitis Symptoms
Acute pancreatitis usually sets in suddenly. Typical symptoms can include severe abdominal pain, fever, nausea, vomiting, and a fast pulse rate.
Chronic Pancreatitis Symptoms
Chronic pancreatitis may present with similar symptoms to acute but on a recurring basis. Symptoms may also include unexplained weight loss and oily stools.
When to Seek Medical Help
Seek medical attention if you experience severe abdominal pain, especially if accompanied by other symptoms such as fever and nausea. It’s vital to get diagnosed and treated promptly, since pancreatitis can lead to serious complications if left unchecked.
Diagnosing Pancreatitis
Getting a definitive diagnosis for pancreatitis involves a few steps.
Medical History and Physical Examination
First, your doctor will want to conduct a thorough medical history and physical examination. This can help them detect any risk factors or signs pointing to pancreatitis.
Laboratory Tests for Pancreatitis
Your doctor may also conduct specific laboratory tests. These tests check the levels of pancreatic enzymes in the blood, which can indicate inflammation if they are unusually high.
Imaging Tests
In some cases, imaging tests such as ultrasound, CT scans, or MRIs may be performed. These can highlight visible changes in the pancreas, such as swelling, which can back up a diagnosis of pancreatitis.
Complications and Consequences of Pancreatitis
Untreated or chronic pancreatitis can lead to several complications over time.
Potential Complications for Acute Pancreatitis
Acute pancreatitis, if severe, can result in life-threatening complications such as kidney failure, diabetes, malnutrition, or even pancreatic cancer.
Long-term Consequences of Chronic Pancreatitis
Chronic pancreatitis can similarly lead to malnutrition and diabetes, as well as create a greater likelihood of developing pancreatic cancer.
Impact on Quality of Life
The recurring pain and discomfort caused by pancreatitis can significantly impact quality of life, limiting activity levels, and potentially causing stress and anxiety about flare-ups.
Treatment Options for Pancreatitis
Treatment for pancreatitis aims to relieve its symptoms and manage any complications.
Medication for Pain Management and Inflammation
Medications can be prescribed to help manage pain and reduce inflammation in the pancreas.
Surgical Interventions
In certain cases, surgery may be warranted to remove gallstones, drain fluid from the pancreas, or remove the pancreas altogether.
Changes to Diet and Lifestyle
In addition to medical treatments, your healthcare team may advise modifications to your diet and lifestyle to help manage your pancreatitis. This can include abstaining from alcohol, quitting smoking, and maintaining a healthy weight.
Managing Diet with Pancreatitis
Nutrition plays a key role in managing pancreatitis.
Pancreas-Friendly Foods
These are generally high in nutrients, lean protein, and low in fats. They include fruits and vegetables, whole grains, and lean proteins like chicken or fish.
Foods to Avoid with Pancreatitis
Try to avoid foods high in fat and sugars, fried foods, and full-fat dairy products as they might aggravate the condition.
Importance of Hydration
Considering the vital role the pancreas plays in digestion, keeping yourself hydrated is crucial. Aim to drink a sufficient amount of water each day.
Living with Chronic Pancreatitis
Living with chronic pancreatitis involves daily life adjustments.
Daily Life Adjustments
These adjustments can range from dietary changes to regularly taking prescribed medications, scheduling regular check-ups with your doctor, and maybe even undergoing therapy or counseling.
Emotional and Psychological Impact
The chronic nature of pancreatitis can lead to emotional and psychological stress. You might find it beneficial to speak with a mental health professional or join a support group to help you cope.
Support for Individuals with Chronic Pancreatitis
Reach out to friends, family, or support groups to help you navigate through the difficult times. There are also professional services available to support you in managing your condition.
Preventing Pancreatitis
There are ways to lower your risk of developing pancreatitis.
Role of Healthy Lifestyle in Prevention
Living a healthy lifestyle by avoiding excessive alcohol, maintaining a balanced diet, and exercising regularly can significantly reduce your risk.
Medical Screening for High-Risk Individuals
If you have a genetic predisposition to pancreatitis, or other risk factors, regular medical screenings can help detect any early signs of the condition, allowing for earlier intervention.
Cutting Down on Alcohol and Smoking
As excessive alcohol consumption and smoking significantly increase the risk of pancreatitis, cutting down or quitting can greatly reduce this risk.
Latest Research and Developments on Pancreatitis
Lastly, there are continuous advancements being made in the research and development of pancreatitis.
New Diagnostic Techniques
New diagnostic techniques are being explored to improve early detection and treatment of pancreatitis.
Potential Treatments Under Investigation
Innovative treatments, including gene therapy and personalized medicine, are under investigation. These potential treatments aim to target the root cause of the disorder, offering hope for more effective treatment strategies in the future.
The Future of Pancreatitis Treatment
While much is still unknown about pancreatitis, the continuous research and development in this field promise improvements in detecting, managing, and treating this complex condition. In the meantime, living a healthy lifestyle and managing existing conditions are the best defenses against pancreatitis.